
The Amide Advantage
Nacuity’s refined, prescription-quality amide, NPI-001, has significant advantages over NAC. NPI-001 is more lipophilic and more easily permeates cell membranes than NAC. In preclinical studies, it has exhibited the ability to cross blood-brain and blood-retinal barriers.
Nacuity is studying the broad clinical potential of a differentiated, purified, prescription-quality, GMP-grade N-acetylcysteine amide (NPI-001). The company’s lead candidate (NPI-001), manufactured using a patented process, is the amide form of N-acetyl-L- cysteine (NAC).
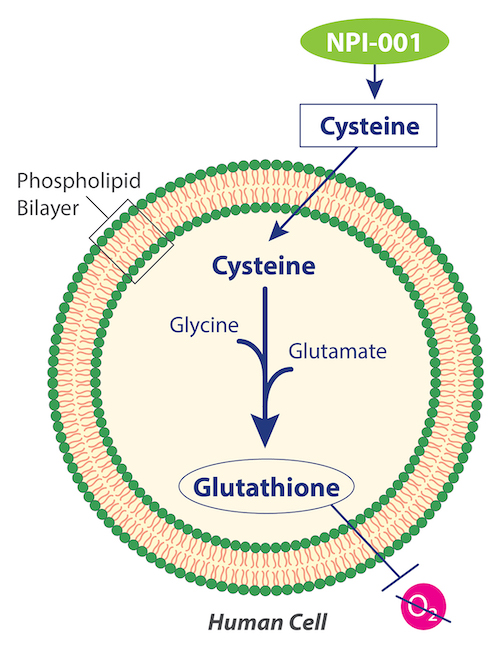
Glutathione
NPI-001 targets cells’ lack of available cysteine, which is required for intracellular biosynthesis of glutathione. Glutathione is the body’s most effective endogenous antioxidant. While it is found in every cell, glutathione cannot penetrate cell walls, thus it cannot be supplemented from outside and it must be biosynthesized inside the cell. The substrates, glutamate and glycine, are often present in cells, but some cells lack sufficient cysteine to make additional glutathione.
NAC
Previous research with NAC has demonstrated its mechanism of donating cysteine to boost glutathione to treat disease. NAC is a well-known, antioxidant moiety that is capable of facilitating glutathione biosynthesis, replenishing glutathione within cells that are undergoing oxidative stress. NAC is approved by numerous regulatory agencies for the treatment of hepatotoxicity caused by acetaminophen overdose, involving replenishment of glutathione in the liver. It is also approved as a mucolytic agent.
NACA Advantage over NAC
Nacuity’s refined, prescription-quality amide, NPI-001, has significant advantages over NAC. NPI-001 is more lipophilic and more easily permeates cell membranes than NAC. In preclinical studies, it has exhibited the ability to cross blood-brain1 and blood-retinal barriers.
NPI-001, if demonstrated safe and effective, has the potential to treat a broad set of diseases and conditions associated with oxidative stress and reduced glutathione levels – such as slowing or stopping disease progression in retinitis pigmentosa patients with functioning cones, regardless of their disease-causing genetic mutation.

Ocular Diseases Involving Oxidative Stress
Nacuity’s antioxidants, if demonstrated safe and effective, have the potential to treat several ocular diseases and conditions associated with oxidative stress and reduced glutathione levels.
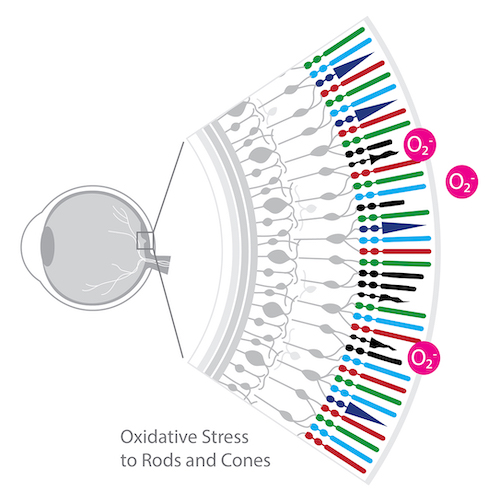
Retinitis Pigmentosa:
Accumulating experimental evidence points to oxidative stress as a pathogenic factor in RP.2 , 3 , 4 , 5 , 6 , 7
- An immunohistochemical study in a RP pig model suggested that the death of rods results in decreased oxygen consumption and hyperoxia in the outer retina resulting in gradual cone cell death from oxidative damage.2
- In a study using the rd1 mouse RP model, a mixture of antioxidants including alpha-tocopherol, ascorbic acid, Mn(III)tetrakis(4-benzoic acid)porphyrin and alpha-lipoic acid improved biomarkers of oxidative stress (protein carbonyl adducts and acrolein staining) and partially preserved cone function.3
- Antioxidant-treated rd10+/+ mice showed preservation of cone function, including a significant increase in photopic ERG b-wave amplitudes. 4
Mutations that cause RP initially lead to rod cell death. After rod photoreceptors die, cone photoreceptors gradually die.8
In a study of RP patients, Campochiaro et al.9 reported a significant reduction in the ratio of reduced glutathione (GSH) to oxidized glutathione (GSSG) in aqueous humor and a significant increase in aqueous protein carbonyl content, compared to control subjects. In contrast, there was no significant decrease in the serum GSH/GSSG ratio or increase in carbonyl content of serum proteins. These data suggest that patients with RP may exhibit ocular oxidative stress, ultimately leading to cone death. Potent antioxidants, therefore, should promote cone survival and function in patients with RP and aqueous GSH/GSSG ratio and protein carbonyl content may provide useful biomarkers.
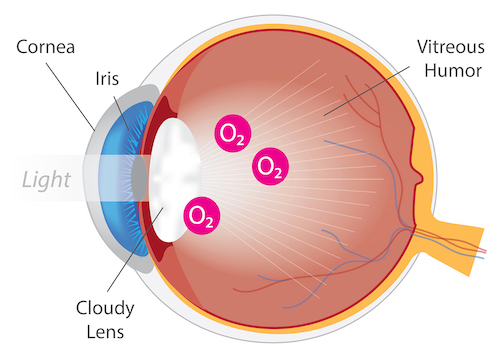
Cataract:
Several nonclinical studies have demonstrated the anticataract activity of NACA in various in vivo cataract models.
Carey et al.10 have shown the efficacy of NACA against L-buthionine-(S,R) sulfoximine (BSO, a glutathione synthesis inhibitor)- induced cataract in wistar rat pups. Also, NACA was shown to inhibit dexamethasone-induced cataract formation by limiting lipid peroxidation and increasing the ratio of GSH/GSSG in rat lens.11 In addition, NACA prevented acetaminophen-induced cataractogenesis in rats.12 Furthermore, NACA decreased severity of selenite-induced cataract in rat pups.13
Nacuity is developing NPI-002, an analog to NPI-001, as an anticataract agent. NPI-002 has demonstrated activity against peroxide- and glucose oxidase-induced cataracts in isolated rat and pig lenses.
Corneal (ocular) cystinosis:
Structures of the eye accumulate cystine crystals14 in patients with cystinosis,15 causing severe photophobia (sensitivity to light), eye pain, damage to the cornea, vision problems, e.g., haziness, foreign body sensation, squinting, band keratopathy, and blepharospasm (involuntary eye closure). Evidence of oxidative stress has been demonstrated in children with cystinosis.16
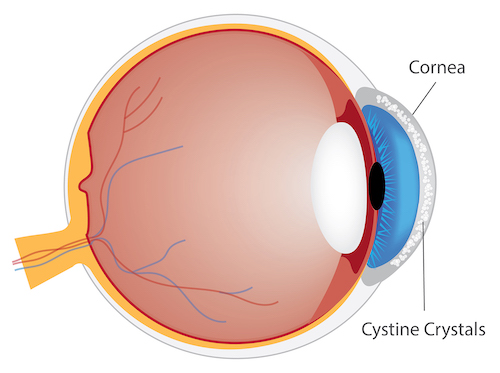
Current cysteine-depletion oral cysteamine therapy does not reach the avascular corneal tissues so it is ineffective in treating ocular (corneal) cystinosis.17 CYSTARAN® and CYSTADROPS® eye drops both contain cysteamine (as the hydrochloride salt). These eyedrop products are indicated for dosing frequently throughout the day, i.e., every waking hour with CYSTARAN® and four times per day with CYSTADROPS®. Both eyedrop products are relatively unstable at room temperature, must be discarded within one week of opening, require frequent dosing, and cause discomfort. In light of the significant issues associated with currently available treatments, the need for effective and tolerable alternative therapies remains.
Nacuity’s antioxidants lack cytotoxicity and increase viability of human cystinotic fibroblast cells in culture. NPI-001 has been shown to deplete cystine from human cystinosis fibroblast cells in culture statistically significantly greater than cysteamine.18

Non-Ocular Diseases Involving Oxidative Stress
Several antioxidants like NAC, lipoic acid, tocopherol, probucol, and Coenzyme QlO have been investigated for their neuroprotective efficacy. Unfortunately, these agents do not cross blood-brain barrier (BBB). BBB permeability is a requirement for any neuroprotective antioxidant. Based on its ability to cross the BBB, NACA has been evaluated for its neuroprotective effect using cell lines and rodent models of neurological diseases/disorders.
Nephropathic cystinosis:
Oxidative stress plays a role in the pathogenesis of cystinosis.16, 19 Indeed, the antioxidant, N-acetylcysteine (NAC, the active ingredient in MUCOMYST®, ACETADOTE® and CETYLEV®) has been shown to improve cystinosis.19
Nacuity’s small molecule antioxidants lack cytotoxicity and increase viability of human cystinotic fibroblast cells in culture. NPI-001 depleted cystine from human cystinosis fibroblast cells in culture statistically significantly greater than cysteamine.18
Heriditary cystatin C amyloid angiopathy (HCCAA):
HCCAA is a rare dominantly inherited disease caused by a leucine to glutamine variant of human cystatin C (hCC). L68Q-hCC forms amyloid deposits in brain arteries associated with micro-infarcts, leading ultimately to paralysis, dementia and death in young adults. To evaluate the ability of molecules to interfere with aggregation of hCC while informing about cellular toxicity, we generated cells that produce and secrete WT and L68Q-hCC and have detected high-molecular weight complexes formed from the mutant protein. Incubations of either lysate or supernatant containing L68Q-hCC with reducing agents glutathione or N-acetyl-cysteine (NAC) breaks oligomers into monomers. Six L68QhCC carriers taking NAC had skin biopsies obtained to determine if hCC deposits were reduced following NAC treatment. Remarkably, ~50–90% reduction of L68Q-hCC staining was observed in five of the treated carriers suggesting that L68Q-hCC is a clinical target for reducing agents.
Reducing agents similar to NAC, NACA and NAC-methyl ester, were evaluated for their effects on oligomerization/dimerization of secreted hCC in vitro. NACA and NAC-methyl ester exhibited approximately 10-fold greater activity compared to NAC20. Based on the favorable bioavailability of the amide, NACA, over the acid, NAC,21 and likely its methyl ester,22 the pursuit of NACA therapy for treatment of HCCAA is warranted.
Gain-of-function mutation in ACOX1, Mitchell Syndrome:
Gain-of-function mutation in peroxisomal acyl-CoA oxidase 1 (ACOX1) is a very rare heterozygous missense variant (p. N237S) disorder characterized by an increase in reactive oxygen species (ROS), chronic loss of axons and progressive loss of nervous system function in pediatric patients. Patients with ACOX1 (p.N237S) exhibit loss of glia, Schwann cells and neurons. The equivalent mutation expressed in fruit flies (Drosophila, da>dACOX1N250S) also exhibited elevated levels of ROS and increased lethality. Feeding mutant flies the antioxidant, NACA, suppressed the neurodegeneration caused by gain-of-function mutation in ACOX1. Similarly, the same mutation in rodents also causes increased ROS in Schwann cells and leads to death of primary Schwann cells in culture. The effects of the mutation are reduced by treatment with NACA resulting in increased survival of Schwann cells.23
A nerve biopsy of the first known patient with the ACOX1N237S mutation revealed a loss of Schwann cells. Similarly, overexpression of hACOX1N237S in cultured rat Schwann cells induced apoptosis, and cell death was suppressed by NACA. Given that NACA was able to counteract the effects of the ACOX1 gain-of-function mutation, antioxidant treatment was considered for patient#1 during a severe disease flare. Since NACA is not approved for use in humans, a related drug, NAC, was used. During a several-month course of NAC treatment, patient#1 had a dramatic improvement in peripheral nerve function. Possibly because NAC does not cross the blood-brain barrier well enough, the patient eventually succumbed to a novel and rapid onset of CNS disease. In honor of patient#1, the investigators named this novel ACOX1-mediated disease “Mitchell Syndrome” (distinct from “Mitchell's disease”, Erythromelalgia).24 Based on these findings, the pursuit of NACA therapy for treatment of Mitchell Syndrome, is warranted.
